Breast augmentation surgery, also known as augmentation mammoplasty, is a common cosmetic procedure that involves the placement of breast implants to enhance the size and shape of the breasts. Breast Enhancement or enlargement is also more popular as a Boob Job.
Dr Mark Doyle offers a number of breast implant types and options to suit you. He is one of the best plastic surgeons in Queensland. He can provide you with a caring, supportive environment and decades of experience to help you achieve your desired result.
What Is Breast Augmentation ?
Breast Augmentation, at a glance
Target area: Size and shape of the breasts
Time off work: 1-2 weeks
Total recovery: 6-weeks
Compression garment: 2 weeks full-time wear, 6 weeks total
Scar position: Along the fold beneath the breast
Breast augmentation is a cosmetic procedure designed to increase and enhance the size and shape of your breasts. This is a very common procedure among women. But, there are a number of things to consider when making the decision to undergo breast enlargement surgery. There are a large number of options with boob job including implant choice and surgical techniques. Dr Doyle will discuss with you all during your initial consultation, depending on the result you are looking to achieve.
Consultation
During your initial consultation at our clinic, Gold Coast Plastic Surgery located on the Gold Coast, Dr Doyle will help you determine what size and shape you would like. After measuring the dimensions of your breasts, He will have you try on a number of trial breast implants. So you can get an idea of what the final results will look and feel like.
Also, he will discuss your surgical options, the operation, risks and recovery from breast augmentation. He will answer any questions you might have about the breast augmentation surgery. You should receive all the information you need to make your decision about whether to go ahead with the surgery or not.
If you are a smoker, you must stop smoking at least three months before surgery, and continue to abstain during recovery. Nicotine causes blood vessels to shrink, compromises the function of red blood cells, and lowers oxygen levels in the blood. Cells must divide and grow in order for wounds to heal. Without adequate oxygen, this process can delay considerably.
Good Candidate
You might be a good candidate for a breast enhancement if your breasts are:
- Mildly sagging
- Flattened
- Low volume
- Uneven or asymmetrical
- Lacking upper pole cleavage
- Pointy with puffy nipples (tuberous breasts)
- Or if you are just wanting to aesthetically change your appearance.
It is very important to communicate with your surgeon before the operation to make sure you have realistic expectations of the outcome.
Want more assistance? Book your initial consultation or take our quiz today to determine if you’re a good candidate for a boob job on the Gold Coast.
What Are The Benefits of Boob Job?
Breast augmentation allows you to modify your breast size, chest proportions, your side profile and potentially the size, shape and location of your nipples (in a procedure called nipple reshaping).
The main benefit of undergoing breast augmentation is changing the way that you look. An enlarged chest will change your body proportions and add balance to your figure. According to a long term study by Clinical Psychological Science, patients displayed increased enjoyment of life and satisfaction after having their physical appearance surgically altered.
Is Breast Augmentation a Major Surgery?
Breast augmentation is a major surgical procedure. It will increase and enhance the size and shape of a woman’s breast. There are a large number of options with breast augmentation, including implant choice and surgical techniques. Dr Doyle will discuss these with you, ensuring you can achieve your desired outcome.
Breast augmentation surgery typically takes under an hour. The location of the incisions depends on your anatomy, goals, and the type of implant you choose. At Gold Coast Plastic Surgery, we make every effort to ensure that your incisions are as small as possible. During breast enlargement, Dr will create a space (or pocket) under the breast. He will put the implant behind or in front of the chest muscle, depending on the look you want to achieve. Most patients receive dissolvable stitches and usually Dr performs it as a day surgery procedure at John Flynn Private Hospital.
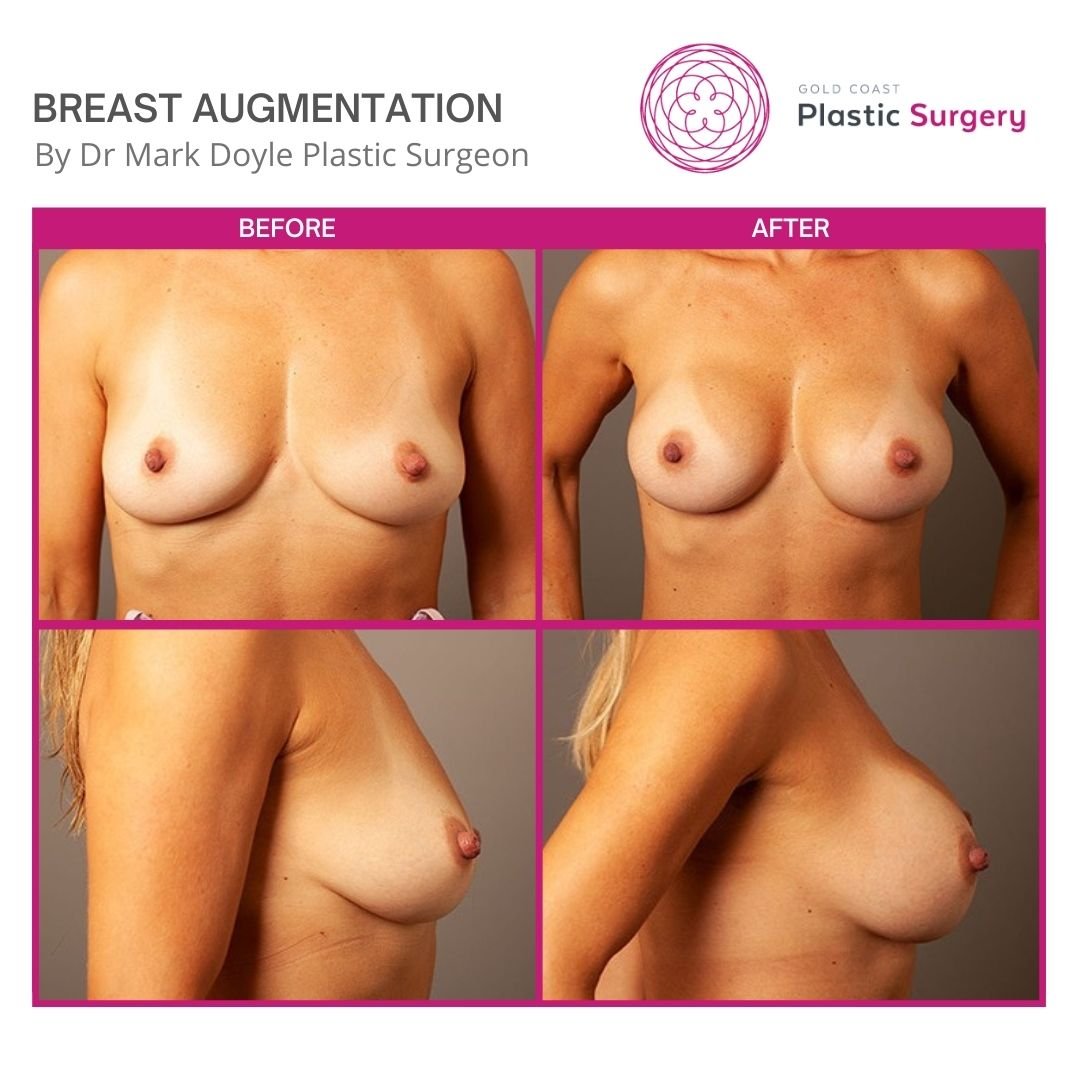
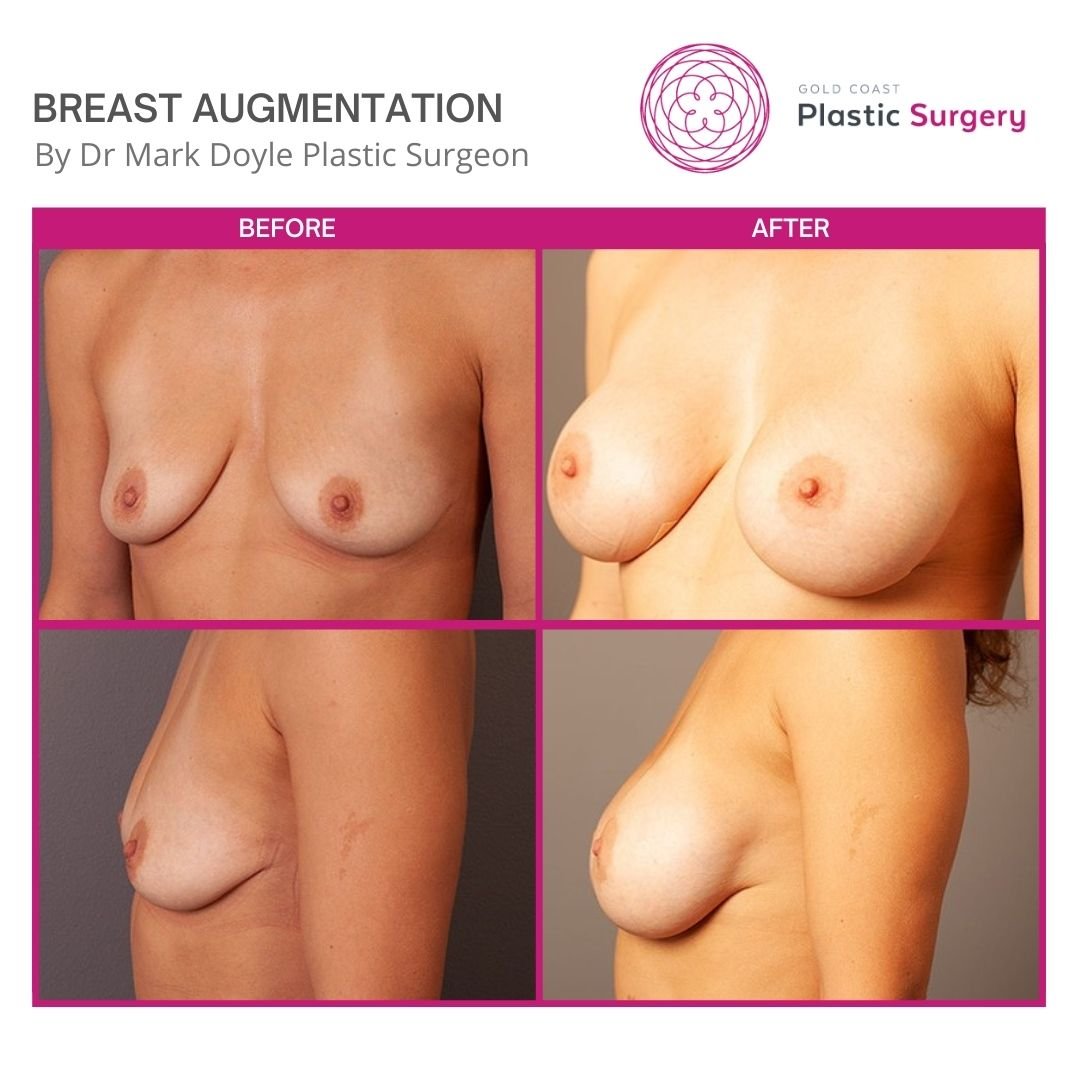
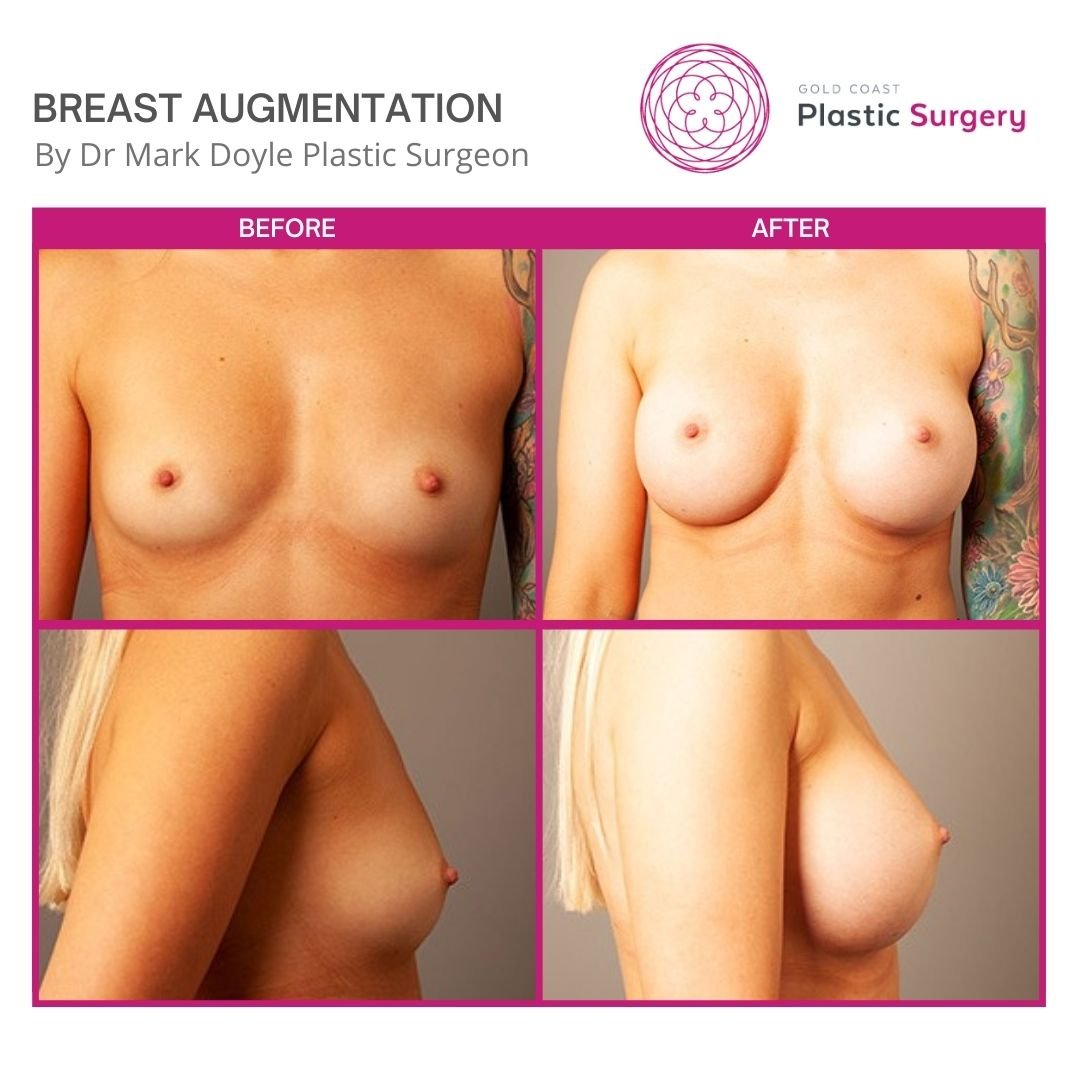
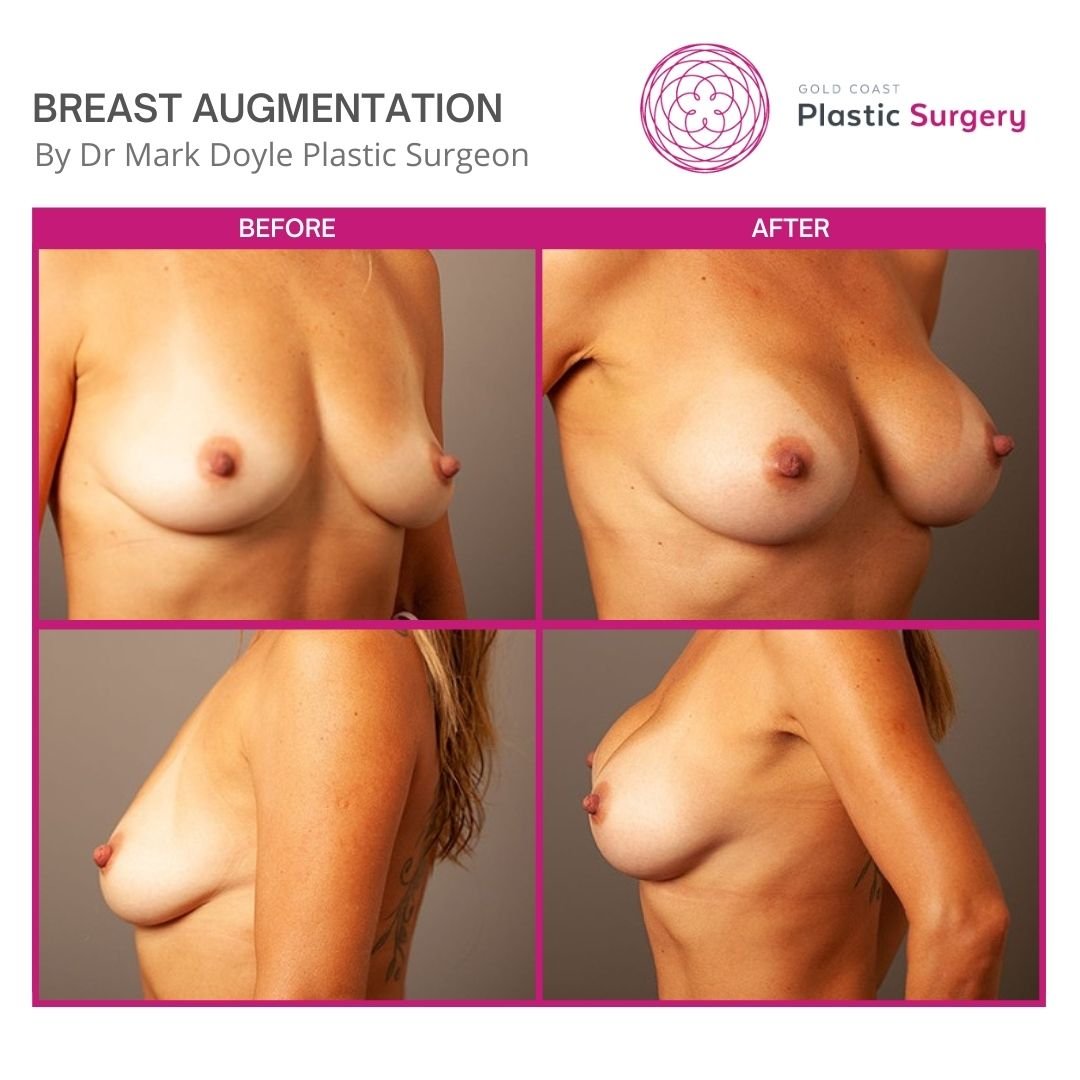
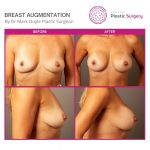
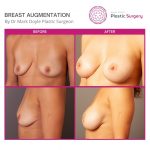
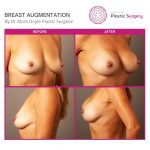
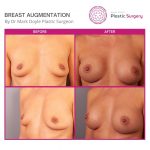
Breast Augmentation Before and After
View all Breast Augmentation Before and After
Breast Augmentation Procedure
During breast augmentation, Dr will create a space (or pocket) under the breast. He will place the implant behind or in front of the chest muscle, depending on the look you want to achieve.
Most patients receive dissolvable stitches and usually, Dr performs it as a day surgery.
1. Surgical General Anaesthesia
Medications are administered for your comfort during the surgical procedure. All surgical procedures are performed under general anaesthesia at an accredited facility. Dr Mark Doyle will recommend the best choice for you.
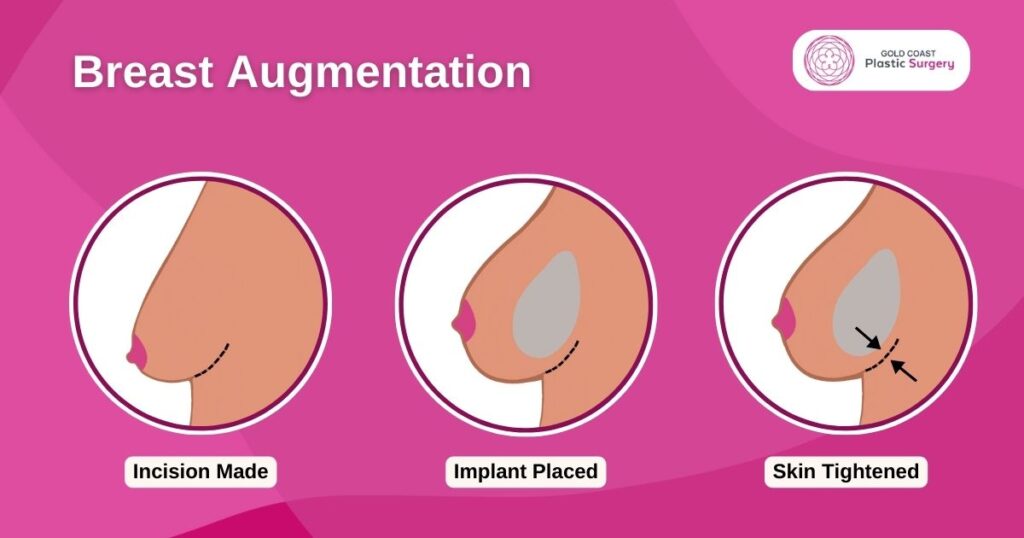
2. Making the incision
Incisions are made in inconspicuous areas to minimise visible scarring. Dr Doyle will discuss with you which incision options are appropriate for your desired outcome. Incisions vary based on the type of breast implant, degree of enlargement desired and your particular anatomy.
3. Inserting and placing the breast implant
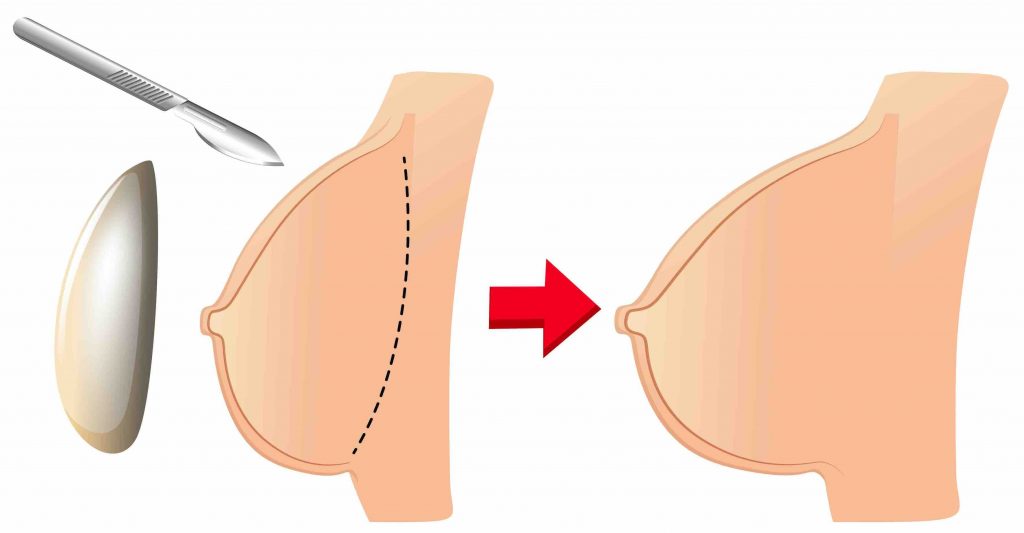
After the incision, Dr will insert the breast implant into a pocket either:
- Under the pectoral muscle (a submuscular placement)
- Directly behind the breast tissue, over the pectoral muscle (a submammary/ subglandular placement)
The method for inserting and positioning breast implants depends on the type of implant, degree of enlargement desired and your body type and Dr Doyle will finalise it before going to the surgery.
4. Closing the incisions
Incisions are closed with layered sutures in the breast tissue. Over time the incision lines will fade. The quality of scar depends on many things, including your genetics, exposure of your body to nicotine and infection.
5. Post-Op recovery
Breast augmentation recovery, a crucial phase in this popular cosmetic procedure, usually lasts up to four weeks. We recommend taking a week off work for effective healing, as most pain subsides within the first week. While temporary discomfort and swelling may persist for a few weeks, it’s important to avoid strenuous exercise and heavy lifting during the entire four-week recovery period for optimal results.
Breast Implants Cost
When considering breast Augmentation surgery, understanding the cost factors and potential insurance coverage is important. Here’s a breakdown of the key aspects to consider:
Medicare Rebate for Breast Augmentation
Medicare rebate for breast augmentation will be available in certain circumstances. However, it’s important to note that breast augmentation is generally considered a cosmetic procedure and may not be covered by Medicare unless it is deemed medically necessary due to congenital deformity, breast reconstruction following mastectomy, or other approved indications. It is advisable to consult with your surgeon and Medicare to determine if you meet the eligibility criteria for a rebate.
Cost Considerations
When contemplating the breast augmentation price, there are several factors to keep in mind. Here’s a breakdown of the key aspects to consider, starting from a base cost of $16,000.
- Surgeon’s Experience: Highly experienced and reputable plastic surgeons may charge higher fees.
- Hospital or Surgical Facility Fees: These fees cover the use of the operating room, nursing staff, and related services.
- Anesthesia Fees: The cost of anesthesia services provided by an anaesthetist.
- Implant Type and Quality: The cost of breast implants can be influenced by various factors, including the type (saline or silicone), brand, size, and specific features of the implants.
- Post Surgery Expenses: It’s important to consider the expenses associated with the post-surgery recovery period, such as medications, follow-up appointments, and supportive garments or bras.
To receive an accurate cost estimate for your breast Augmentation surgery, it is advisable to schedule a consultation with a specialist plastic surgeon. During the consultation, the surgeon will assess your unique case and provide a personalised cost breakdown based on your specific needs and the required procedures.
FAQs
How Long Do Breast Implants Last?
The average lifespan of older breast implants is about 20-25 years. Newer implants have not been available for this length of time but it is expected that they will last longer than the original implants. However, this does vary from person to person and depends on which type—and where—the implant is placed. The quality of the implant is also a factor in its lifespan. Dr Mark only uses the highest quality Motiva breast implants.
How Do I Choose the Size of My Breast Implants?
Dr Doyle uses Crisalix 3D imaging technology in all his breast augmentation consultations. This allows you to trial different implants sizes and shapes to imagine how they will fit with your body shape. This 3D before-and-after technology gives you and Dr Mark a preview of the expected cosmetic results from your breast augmentation procedure.
I use 3D planning tools on all breast patients to accurately assess breast volume and asymmetry prior to surgery and to allow the patients to have more input into the results they wish to achieve with their surgery. 3D simulation of results using different size implants can be invaluable in making an informed decision regarding breast size,” says Dr Doyle.”
Is It Possible to Combine Multiple Plastic Surgery?
Yes. Breast augmentation surgery can combine with a Breast Lift to address sagging tissue. This procedure is Breast Lift with Implants Surgery. It’s one of Dr Doyle’s signature procedures. Also breast lift before and after photos will give you an idea about the procedure.
This procedure also combines well with Tummy Tuck surgery for total body change. It is incredibly popular with women who have finished their families and want to restore their pre-pregnancy bodies.
Dr Doyle can perform Breast Augmentation at the same time with Rhinoplasty procedure as well as other facial surgeries.
Will My Breasts Look Natural After a Breast Augmentation?
While Dr Mark strives to achieve natural-looking results for his breast augmentation patients, the outcome is dependent on your goals for the surgery.
“My surgical technique and implant choice both in terms of projection, size and round vs teardrop shapes, will change depending on whether you desire a natural or fake look. The positioning of breast implants above or below the pectoral muscles will also affect the final result,” says Dr Doyle.
Can I Get Really Large Implants?
Dr Doyle does not use implants larger than one litre in size. You can discuss your size options in a consultation session.
“For those patients considering having larger breast implants to lift the breasts, I would advise them that having larger implants will increase the risk of the implants drooping due to gravity. A breast lift is much more likely to give them a good long term result. Larger heavier implants are much more likely to give rise to complications and the need for further surgery,” says Dr Mark.
Do Breast Implants Drop?
Implants shift and wear over time due to the natural movement of your body. Larger implants and therefore, heavier implants, are more likely to drop with time. Pregnancy, breastfeeding and weight changes will all influence the position of the implants. This means you will have to replace your implants at least once if you want them for life. You should always ensure you visit a plastic surgeon who uses top quality products.
Do I Need to Wear a Bra After Breast Augmentation?
A post-operative bra is given to patients to wear for the first six weeks. This surgical garment supports the breasts and promotes proper healing. It is recommended that patients refrain from driving for at least two weeks after undergoing breast augmentation surgery and avoid partaking in rigorous exercise for at least six weeks.
Can I Breastfeed After Breast Augmentation?
All breast surgery procedures have the potential to affect the nerves and ducts within the breast, which impacts lactation. Breast implants placed below the muscle usually have less effect on milk production than implants placed above the muscle.
It is usually possible to breastfeed after breast augmentation. The type of surgery and in particular, the incisions used for your surgery, can impact your ability to breastfeed.
This is something you must consider prior to surgery. If you are planning on having children, you need to weigh up the possibility you won’t be able to breastfeed your child.
Which Type of Breast Implant Is Right for Me?
There are three main types:
- Saline: Filled after insertion with smaller incisions, but some find them less natural.
- Silicone: Preferred for a natural look and feel, though ruptures require prompt attention.
- Gummy bear: Similar to silicone but more stable, with silicone staying in place if ruptured.
Dr. Doyle will discuss these options and sizes during your appointment, allowing you to try different sizes with a specialized bra for a realistic preview of your results.
What Are the Risks of Breast Augmentation?
Modern breast enlargement surgery is low risk. There is, however, no such thing as risk-free surgery. The important thing is to understand all of the potential risks and take the appropriate steps in order to avoid them. Any surgical procedure carries some risk of infection, severe bruising, or reaction to anaesthesia.
In the case of breast augmentation surgery, there is also the possibility of complications related to the breast implant, such as rupture, rippling, or capsular contracture. Risks include:
- Capsular contracture (a tightening of the scar tissue which can make the breast feel hard and can distort the shape of the breast implant).
- Changes in nipple and breast sensation (usually temporary).
- Breast pain
- Rare implant leakage or rupture
Am I too old to undergo breast augmentation surgery?
While most breast augmentation patients tend to be in their 20s or 30s, many women choose to have implants inserted in their 40s and 50s. Regardless of your life stage, if you feel that you would benefit from breast implants, schedule a consultation before you decide that you’re not eligible.
What is recommended is that you wait until after you’ve had children to schedule this type of surgery. This is not to say that having breast implants will affect future pregnancies or your ability to breastfeed though. There is, however, a chance that your results will be affected by pregnancy. The choice is yours.
Can I Undergo Breast Augmentation if I Have Sagging Skin?
Sagging skin, or ptosis, shouldn’t deter you from undergoing breast augmentation surgery. If the sagging is severe, the procedure may need to be combined with a breast lift to achieve a more favourable result. This procedure is called a breast lift with implants surgery. If any excess skin is not removed, the implants will only cause the breasts to sag even further. Dr can advise you whether a lift will also be necessary once your breasts and goals have been evaluated.
Is There a Loss of Nipple Sensation if You Get Implants?
The implant placement method influences your risk of sensation loss. Incisions made under the areola pose a higher risk of numbness, whereas incisions under the breast fold typically result in less pronounced numbness. Complete loss of sensation is rare. Following the healing process, full nipple functionality can be restored. Dr Doyle will explain his techniques to minimise the risk of complete sensation loss.
Book a consultation
Dr Mark Doyle offers breast augmentation surgery to all patients in Brisbane, Sunshine Coast and Gold Coast. To find out if breast surgery is right for you, book a consultation with him. Patients from all around Queensland and Northern Suburbs of NSW are welcome to visit us at Gold Coast Plastic Surgery on the Gold Coast.
About Dr Mark Doyle FRACS (Plast) – Queensland Plastic Surgeon
Servicing patients in Gold Coast, Brisbane, Sunshine Coast, Cairns and New South Wales NSW – Northern Rivers, Byron Bay, Ballina, Lismore and more.
Dr Mark Doyle is a Specialist Plastic Surgeon with over thirty years of experience performing Breast, Body, Face and Nose surgery. Dr Doyle is a fully qualified Specialist Plastic Surgeon with 30+ years of experience. He has completed all required training and only carries out approved surgical practices. There are absolutely NO undertrained doctors or cosmetic doctors acting as surgeons in our clinic.
As a highly esteemed plastic surgeon, Dr Mark is committed to achieving the best possible results for all his breast, body, face and nose patients, both men and women.